COVID-19 pandemic has inadvertently, though fortunately, brought the conversations around health, immunity, and nutrition centre-stage. Often the importance of a healthy lifestyle is ignored or taken for granted, especially in resource-poor settings where the major focus is on livelihoods. Undernutrition (wasting and stunting) being a more noticeable consequence of COVID-19 pandemic, has been highlighted, and rightly so, widely. But what is equally important to understand and discuss is how COVID-19 is exacerbating the other ensuing burden of overweight-obesity especially in Low and Middle-Income Countries (LMICs) like India. Sadly, overweight-obesity as a public health nutrition issue garners much attention neither from the masses nor the policymakers. World Health Organisation (WHO) rightly opined, “Obesity although being amongst today’s most blatantly visible public health problem, yet remains the most neglected”.
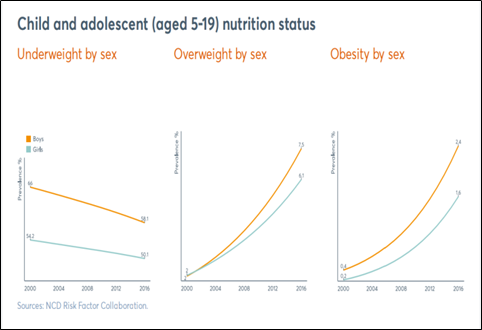
The Global Nutrition Report (GNR, 2020) notes the alarming rise in obesity prevalence among Indian children – 2.4 % boys and 1.6 % girls in the age group of 5-19 years – (see figure 1) in addition to a huge but declining undernutrition burden. Similar rising trends have been shown for the adults (see figure 2). Forecasts portend that the prevalence of overweight will be more than double among Indian adults aged 20–69 years between 2010 and 2040, while the prevalence of obesity will triple. Specifically, the prevalence of overweight and obesity will reach 30.5% and 9.5% among men, and 27.4% and 13.9% among women, respectively, by 2040. The largest increase in the prevalence of overweight and obesity between 2010 and 2040 is expected to be in older ages and in rural areas.
But why should we worry about obesity?
Obesity is a major pro-inflammatory risk factor implicated in the onset of non-communicable diseases like heart problems, diabetes, hypertension, some cancers, etc. It also compromises lung function and may lead to musculo-skeletal disorders. Two major individual behaviour related causes associated with rising overweight-obesity are poor diets (both quality and quantity matters!) and reduced physical activity. However, several other reasons like genetics, poor awareness, hormonal imbalances, reduced sleep, high-stress levels, environmental pollutants, co-morbidities which restrict movement have also shown to be associated with obesity. In addition, there are implicit socio-economic and cultural factors like weak policies, poverty, lack of education, cultural beliefs, sub-optimal food environment, etc. which may fuel obesity further.
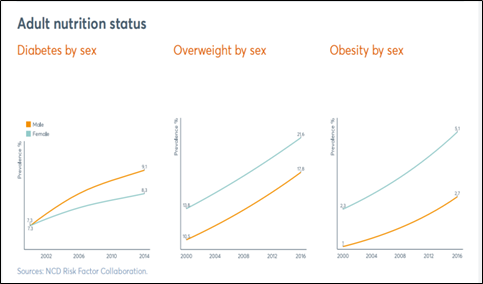
Source: Global Nutrition Report (2020)
Some examples are discussed below. Families experiencing a devastating loss of livelihoods or drop in incomes also reported limited access to and affordability of food (especially, the healthy sources), essential medicines, and basic healthcare. Recently released State of Food Security and Nutrition in the World 2020 (SOFI 2020) report suggests that on an average healthy diet are five times more expensive than the diets which meet only the energy needs. They have estimated about 300 crore people in the world are unable to afford nutritious foods. Rapid surveys and few studies indicate that nation-wide lockdown has led to a sharp decline in physical activity duration of Indians (especially among children) along with an increased frequency of snacking. High-quality nutrition foods, like fresh fruits, vegetables, dairy, eggs, etc., have become challenging to source given their quickly perishable nature and high prices. Further, services like the regular growth monitoring, immunization services for the children, provision of Iron-Folic Acid (IFA) tablets, Integrated Child Development Services (ICDS) take-home rations & hot-cooked meals, mid-day meals in the schools, etc. were also disrupted to a large extent. In India, the lockdown coincided with the peak harvesting time, which further disturbed the entire process of the food system chain and resulted in a lack of provision of nutritious and healthy diets to people.
The World Vision International (WVI) 2020 rapid assessment analysis of several South Asian countries, including India, revealed that 51% of Indian households (49% in urban) were purchasing food of lesser quality (largely, highly processed foods with longer shelf lives and poor nutritional values). The halt of transportation services in the nation resulted in the unavailability of fresh fruit & vegetables, and an elevated demand & consumption of affordable packaged foods further added to increased chances of obesity. Along with this, panic buying and hoarding by those who could afford it deprived the vulnerable sections of even the normal diets, let alone the healthy and nutritious foods.
The good news is that most of these are modifiable and if corrected, can go a long way in helping India check this ‘weighty’ issue. We propose a P-R-I-C-E to pay to rein in this stubborn form of malnutrition, i.e., overweight-obesity.
- P- Policy– Innovative policies to promote healthy diets and physical activity through the life-course are needed urgently. An important factor while planning any policy is to increase the affordability of healthy diets and bring down the cost of nutritious foods. The SOFI 2020 explains that “cost drivers of these diets are seen throughout the food supply chain, within the food environment, and in the political economy that shapes trade, public expenditure and investment policies”. Integral components of such policies include, but not limited to, strengthening of food systems, repairing the food environment, focusing on nutrition security, reducing food loss and wastage, demarcated financing, robust and transparent accountability, leadership, governance to propel people and pocket-friendly nutrition policies, designing and implementing effective multi-sectoral partnerships (especially in sectors like trade, environment, education, agriculture, public health, nutrition, urban/rural development, food processing, etc). Some examples of such policies that may help foster behavioural change towards healthy diets include taxation on unhealthy food and beverages, front-of-pack traffic light nutrition labelling, reduction of advertising of junk food and beverages to children, etc. Another impactful cost-effective policy intervention, especially with respect to tackling multiple forms of malnutrition, is the promotion of exclusive breastfeeding (EBF) for the first 6 months. Sadly, only about 55% of our under 6-month-olds are exclusively breastfed. This is a huge opportunity as EBF reduces childhood obesity risk by up to 25% as per the WHO.
- R- Research – The importance of strengthening the evidence base to guide policy towards action on the ground cannot be underscored enough. Research needs will also prompt collaboration among scientists across all disciplines to advance this challenging research agenda given the high potential for translation and impact on public health, e.g. Consortiums and expert groups like Standing Together for Nutrition (STfN), EAT-Lancet group, Global Burden of Disease (GBD) consortium, etc. Research helps to exchange ideas and stimulate the development & adoption of new and innovative strategies that can be contextually applied to the prevention and treatment of multiple forms of malnutrition. Increased investments in all types of research to improve health are needed to turn back the tide of obesity.
- I- Industry – The Lancet Commission on Obesity blamed the food industry, which gorges populations, on empty calories while misusing land, energy and other resources. The 43-member panel pointed to the generous financial resources and political clout of the food industries which helps them to lobby for decisions prioritizing profits over public health. The industry-funded research often entails bias and conflict of interest which need to be recognized and combatted. One of the most cited ways to curb the influence of food industry tactics is to limit junk food availability and advertising especially targeted to children and caregivers.
- C-Capacity building– Poshan Abhiyaan, India’s flagship national nutrition mission also embodies this but more action and innovation is needed to embrace rapidly changing needs in the field, data collection methods, robust indicators to assess nutrition security, validation of new tools, etc. The cadre of public health nutrition professionals (the whole spectrum from advisors, mentors, researchers to frontline workers) needs a lot of nourishment and nurturing in form of skill-building courses, training sessions, exchange programs, appropriate methodology workshops, etc.
- E- Empower – Local tradition of consuming locally available seasonal foods with high fibre and mineral content has been exchanged for processed foods and sugar-sweetened soft drinks even in remotest of places. Screen time, especially of the young ones, has skyrocketed in the past decade. The awareness-building campaigns by communities, NGOs and government should run in parallel to other nutrition schemes/programs to help people make informed choices. Merely providing carbohydrate-rich sources with minimal micronutrients and protein may result in imbalances in nutritional status, which in turn predispose to early onset of metabolic diseases in later life. The Government announced 1.7 trillion rupees (USD 22.6 billion) relief package under the PM Garib Kalyan Yojana to take care of food security measures for the poor. Additionally, distribution of free provision of 5kg of rice/wheat per person, 1 kg of pulse per household along with free cooking gas monthly for three months have also been proposed. Such nutrition-sensitive social protection schemes will also be central to increase the purchasing power and affordability of healthy diets of the most vulnerable populations.
In summary, all forms of malnutrition are unacceptable, but what will be even worse is trying to use siloed approaches to tackle one versus the other. As explained above, a healthy life can go a long way in ensuring the productivity of an individual as well as the economic growth of the nation. This will need concerted efforts from all individuals, communities, and governments. We often say ‘Rome was not built in a day‘ to highlight the importance of incremental steps in getting the desired outcome. So, let us all muster our passionate motivations, correct methods, and positive mindset to contribute to the best of our capabilities in reversing the obesity epidemic in India.
Swasth Bharat, Suposhit Bharat!
Disclaimer: The views expressed in this article are of the author solely. TheRise.co.in neither endorses nor is responsible for them.





Pingback: COVID-19 Vaccine: Who First? - by Anviti Mishra - TheRise.co.in
Pingback: Nai DISHA: To end TB - Society - TheRise.co.in TheRise.co.in
Pingback: Investigating Hunger concerns of India - TheRise.co.in